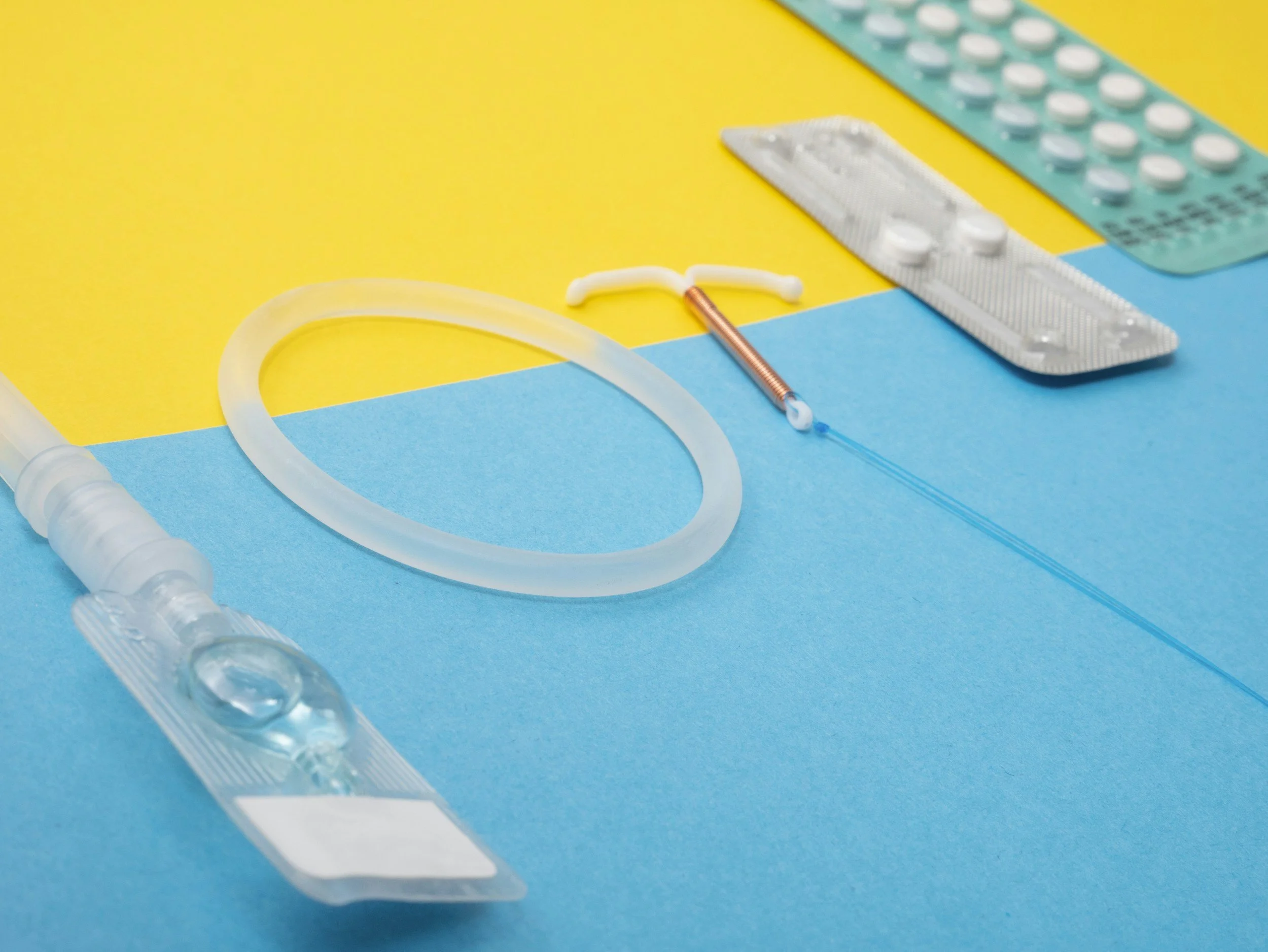
Breaking Down Contraception: A Guide to Birth Control Methods
Choosing the most effective birth control method is essential for managing reproductive health. Understanding how different birth control options work helps individuals make informed decisions.
Common birth control methods include hormonal methods (birth control pills, contraceptive patches, contraceptive rings, and injectable contraceptives), barrier methods (male and female condoms, diaphragms, and cervical caps), long-acting reversible contraception (IUDs and implants), sterilization (tubal ligation and vasectomy), and natural methods (fertility awareness-based methods and the withdrawal method).
Abstinence is the only method that guarantees 100% effectiveness in preventing pregnancy and sexually transmitted infections when practiced consistently. However, it might not be practical for everyone. Keep reading to explore the range of available birth control options to find out which is best for you!
What is the 100% Most Effective Birth Control Method?
The 100% most effective birth control method is abstinence, which involves refraining from any sexual activity that could lead to pregnancy. Unlike other contraceptive methods, abstinence eliminates the possibility of pregnancy altogether, making it the most reliable form of birth control when practiced consistently and correctly. This is due to there being no chance of sperm coming into contact with an egg, thus preventing conception.
Abstinence is not only effective in preventing pregnancy but can also protect you from sexually transmitted infections (STIs) when practiced consistently. While abstinence may not be a feasible option for everyone, especially those in sexually active relationships, it remains the only method that guarantees complete avoidance of pregnancy and STIs.
Additionally, abstinence can be an empowering choice for individuals who prioritize their physical, emotional, or religious beliefs above engaging in sexual activity. Overall, abstinence offers unparalleled effectiveness in preventing pregnancy and STIs, making it a valuable option for those seeking reliable contraception. However, there are still viable options for those not wishing to abstain.
Which Birth Control Method Has the Least Side Effects?
If you want to use birth control, you likely also want to use the method with the least amount of potential side effects. The best choice for you will depend on individual health, preferences, and medical history. However, certain methods are generally associated with fewer side effects than others and are, therefore, more favorable.
Non-hormonal contraceptives like barrier methods (such as condoms and diaphragms) and copper IUDs typically have minimal systemic side effects because they do not introduce hormones into the body. Barrier methods work by physically preventing sperm from reaching the egg, while copper IUDs create an inhospitable environment for sperm, thus preventing fertilization.
Among hormonal methods, progestin-only contraceptives, such as the progestin-only pill (mini-pill), hormonal IUDs, and contraceptive implants, are often preferred by individuals seeking methods with fewer side effects. These methods contain only progestin hormone, which tends to have fewer systemic side effects compared to combined hormonal contraceptives (containing both estrogen and progestin).
However, it's essential to note that individual responses to hormonal contraception can vary, and some people may still experience side effects such as irregular bleeding, mood changes, or changes in libido. Consulting with a healthcare provider can help determine the most suitable birth control method based on individual needs and considerations.
Hormonal Methods
Oral Contraceptives
Oral contraceptives, commonly known as combination birth control pills, are a hormonal method of contraception. They contain synthetic versions of the hormones estrogen and progestin, which work together to prevent pregnancy. These hormones primarily function by suppressing ovulation, which is the release of an egg from the ovary, thereby preventing fertilization.
Additionally, oral contraceptives thicken cervical mucus, making it more difficult for sperm to reach the egg, as well as thin the uterine lining, reducing the likelihood of implantation. Taken daily as directed, oral contraceptives are highly effective at preventing pregnancy when used correctly, offering individuals a convenient and reversible method of birth control.
Contraceptive Patch
Contraceptive patches are another hormonal birth control method that delivers synthetic hormones through the skin to prevent pregnancy. These patches contain both estrogen and progestin hormones, similar to combined hormonal contraceptives like birth control pills. The hormones are absorbed directly into the bloodstream through the skin, where they work to inhibit ovulation, thicken cervical mucus to impede sperm movement, and thin the uterine lining to prevent implantation.
Users typically apply a new patch once a week for three weeks, followed by a patch-free week to allow for withdrawal bleeding. Contraceptive patches offer convenience and effectiveness when used correctly.
Contraceptive Ring
A contraceptive ring is a small, flexible ring that is inserted into the vagina, where it continuously releases hormones to prevent pregnancy. Typically, these rings contain both estrogen and progestin, allowing for the inhibition of ovulation. This method offers the convenience of long-acting contraception without the need for daily administration.
However, like other hormonal methods, contraceptive rings may have potential side effects such as irregular bleeding, breast tenderness, or mood changes, which vary depending on individual factors.
Injectable Contraceptives
Injectable contraceptives, or birth control shots, are a hormonal method of contraception as well. They contain progestin, a synthetic form of the hormone progesterone that helps block sperm and prevent pregnancy.
Administered by a healthcare provider every few months, typically every 13 weeks, injectable contraceptives offer long-lasting protection against pregnancy with a high efficacy rate. While generally safe and effective, they may have side effects such as irregular bleeding, weight gain, and mood changes, which vary among individuals.
Barrier Methods
Male Condoms
Male condoms are a popular barrier method of birth control, as they tend to be effective, accessible, and affordable. Made of thin latex or polyurethane, condoms are worn over the penis to create a physical barrier that prevents sperm from entering the vagina during intercourse.
When used correctly and consistently, they can be highly effective in offering protection not only against pregnancy but also against STIs. Condoms are readily available without a prescription, easy to use, and have minimal side effects. Additionally, they are one of the few birth control methods that provide dual protection, making them a versatile option for individuals and couples.
Female Condoms
A female condom is a barrier birth control method designed to be worn inside the vagina to prevent sperm from entering the uterus during intercourse. Made from polyurethane or nitrile, they consist of a flexible ring at the closed end and a larger ring at the open end.
The closed end is inserted into the vagina, covering the cervix, while the larger ring remains outside the body, providing external protection. When properly placed, female condoms can also provide protection against STIs and greater control over contraception for individuals who may not be comfortable using male condoms.
Diaphragm
A diaphragm is a barrier method of birth control that is inserted into the vagina to cover the cervix and block sperm from entering the uterus. Made of flexible silicone or latex, it is a physical barrier preventing sperm from reaching the egg.
Before intercourse, it must be filled with spermicide (a chemical substance that is available over-the-counter) and inserted deep into the vagina, where it remains in place during sexual activity. It is reusable and can be left in for up to 24 hours, providing continuous protection against pregnancy. While effective when used correctly, it requires proper fitting and insertion techniques for optimal efficacy.
Cervical Cap
A cervical cap is designed to cover the cervix and help prevent pregnancy. The cap is made of silicone or latex and is inserted into the vagina and placed over the cervix before sexual intercourse. The cap creates a barrier that blocks sperm from reaching the egg, thus preventing fertilization. Like a diaphragm, is typically used with spermicide to increase effectiveness.
Long-Acting Reversible Contraception (LARC)
Intrauterine Devices (IUDs)
Copper IUD
Copper intrauterine devices (IUDs) are a form of long-acting reversible contraception (LARC) that provide highly effective birth control for an extended period. Once inserted into the uterus by a healthcare provider, copper IUDs can prevent pregnancy for up to 10 years.
Unlike hormonal methods, copper IUDs do not contain any hormones, making them suitable for individuals who prefer non-hormonal contraception. They work by releasing copper ions, which are toxic to sperm, thus preventing fertilization. Copper IUDs offer convenience and peace of mind, as they require minimal maintenance once inserted and can be removed at any time if pregnancy is desired.
Hormonal IUD
Hormonal IUDs are a form of LARC that offers effective birth control for an extended period as well. A healthcare provider inserts these T-shaped devices into the uterus, where they continuously release a low dose of progestin hormone. This hormone thickens cervical mucus, inhibiting sperm movement, and thins the uterine lining, preventing implantation.
Hormonal IUDs can provide contraception for up to three to seven years, depending on the specific brand. Their long-term effectiveness, convenience, and minimal user effort make them a popular choice for individuals seeking reliable birth control without daily maintenance.
Implants
Implants are a form of birth control that is considered highly effective for a longer period of time. These small, flexible rods are inserted under the skin of the upper arm and release progestin hormone, preventing pregnancy by inhibiting ovulation, thickening cervical mucus, and thinning the uterine lining.
One of the significant advantages of implants is their long-lasting effectiveness, typically providing contraception for up to three to five years, depending on the specific type. This makes implants a convenient option for individuals seeking reliable birth control without the need for daily administration or frequent healthcare visits.
Sterilization
Tubal Ligation (For Women)
Tubal ligation, commonly referred to as "getting one's tubes tied," is a surgical sterilization procedure for individuals seeking permanent contraception. During tubal ligation, the fallopian tubes are either cut, sealed, or blocked to prevent eggs from traveling from the ovaries to the uterus, thereby preventing fertilization.
This procedure is highly effective at preventing pregnancy and is considered a permanent form of birth control. While it is possible to reverse tubal ligation through surgery, the procedure is complex and not consistently successful, so individuals should carefully consider their decision before undergoing this irreversible sterilization method.
Vasectomy (For Men)
A vasectomy is a permanent sterilization method for men seeking long-term contraception. During the procedure, the vas deferens, the tubes that carry sperm from the testicles to the urethra, are surgically cut or blocked to prevent the release of sperm during ejaculation. As a result, sperm cannot mix with semen, effectively preventing pregnancy.
Vasectomies are a highly effective and reliable form of birth control, with a success rate of 99.95%. While considered a permanent method, vasectomy reversal procedures are available but may not always restore fertility. It's important for individuals considering a vasectomy to understand its permanence and implications before undergoing the procedure.
Natural Methods
Fertility Awareness-Based Methods
Fertility awareness-based methods (FABMs) are natural birth control methods that involve tracking menstrual cycles and identifying fertile days to avoid or achieve pregnancy without the use of hormones or devices. By monitoring biological markers such as basal body temperature, cervical mucus, and menstrual cycle length, individuals can accurately identify fertile and infertile days.
FABMs empower individuals to understand their reproductive health and make informed decisions about family planning. While FABMs offer a hormone-free and non-invasive option for contraception, they require commitment, consistency, and accurate tracking to be effective, making them suitable for individuals comfortable with a natural approach to birth control.
Withdrawal Method
The withdrawal method, also known as the "pull-out" method, is a natural birth control approach that involves the male partner withdrawing the penis from the vagina before ejaculation to prevent sperm from entering the female reproductive tract. This method relies on timing and self-control rather than the use of contraceptives or devices.
While it is readily accessible and cost-effective, the withdrawal method requires precise timing and self-discipline to be effective, and it has a relatively high failure rate compared to other contraceptive methods. Therefore, it may not be the most reliable option for preventing pregnancy.
Final Thoughts
Overall, abstinence stands as the 100% most effective birth control method, providing complete avoidance of pregnancy and sexually transmitted infections when consistently practiced. Despite its efficacy, abstinence may not be feasible for everyone. Thus, understanding the various types of birth control methods is crucial for informed decision-making.
Hormonal methods like the birth control pill offer convenience but may come with side effects. In contrast, non-hormonal methods like barrier contraception and the copper IUD provide alternatives with fewer systemic effects.
Ultimately, selecting the most suitable method depends on individual preferences, health considerations, and lifestyle factors. By exploring the range of contraceptive options available, individuals can make empowered choices to promote their reproductive health and disease control.
Frequently Asked Questions
What are five methods of birth control?
Five standard methods of birth control include the following:
Oral contraceptives, commonly known as birth control pills, are taken orally to prevent pregnancy by inhibiting ovulation or thickening cervical mucus.
The male condom is a barrier method that prevents sperm from reaching the egg.
Intrauterine devices (IUDs) are small, T-shaped devices inserted into the uterus to prevent pregnancy by altering the uterine environment.
Depo-Provera injections are hormonal injections administered every three months to prevent ovulation.
Tubal ligation, or sterilization for women, involves blocking or sealing the fallopian tubes to prevent eggs from reaching the uterus.
These methods offer diverse options for individuals to choose the most suitable form of contraception based on their needs and preferences.
What are the three most effective forms of birth control?
Three of the most effective forms of birth control are sterilization, intrauterine devices (IUDs), and hormonal implants. Sterilization procedures, such as tubal ligation for women or vasectomy for men, are permanent methods that prevent pregnancy by blocking the fallopian tubes or vas deferens, respectively. IUDs, both hormonal and non-hormonal, are highly effective long-term contraceptives that are inserted into the uterus. Hormonal implants, inserted under the skin, release hormones to prevent ovulation and thicken cervical mucus, providing long-lasting contraception.
This article has been reviewed by our editorial board and has been approved for publication in accordance with our editorial policy.
Main image credit: Reproductive Health Supplies Coalition / Unsplash
The information provided in this article is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.